FORUM SYMPOSIUM - ROBOTIC
2nd EAORL-HNS, 2nd CE-ORL, 27-30 April 2013, Nice-Acropolis
27/04/13 - 16:00 - 17:30 - ROOM MEDITERRANEE 3
Session: FORUM STOCKTAKING DEVICES: ROBOTIC
FORUM SYMPOSIUM
„ROBOTIC“
Invited speakers:
O. Sterkers (F), I. Klapan (CRO), M.D. Caversaccio (CH), O. Madjani (D),
T. Klenzner (D), Y. N'gyjen (F), S. Verges (F), Ph.C. Lombard (F)
Instructional Course RHINOLOGY 2 N°3
2nd EAORL-HNS, 2nd CE-ORL, 27-30 April 2013, Nice-Acropolis
RHINOLOGY - INSTRUCTIONAL COURSES
27/04/13 - 14:00 - 15:30 - ROOM RISSO 6
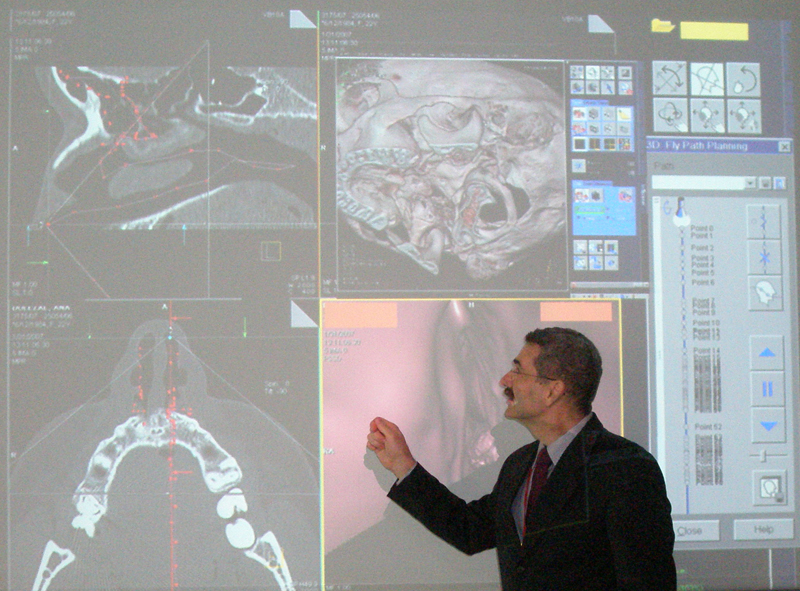
Chairperson: Professor Ivica Klapan, MD, PhD
Zagreb and Osijek University Schools of Medicine, Croatia, and Klapan Medical Group Polyclinic, Zagreb, Croatia, Ilica 191A, HR-10000 Zagreb, Republic of Croatia poliklinika.klapan@vodatel.net
Computer integrated surgery with application of advanced virtual reality (VR) techniques
in interactive virtual rhino-endoscopy/virtual surgery (VS) navigation operation systems
in interactive virtual rhino-endoscopy/virtual surgery (VS) navigation operation systems
The need of a more precise identification of the pathologic process extent as well as of the fine elements of intracranial anatomic features is often experienced in diagnostic process and during many operations in the nose, sinus, orbit and base of the skull region. In two case reports, the methods used in diagnostic work-up and surgical therapy in the nose and paranasal sinus region are described. Besides baseline x-ray, multislice computed tomography and magnetic resonance imaging scans, the techniques of operative field per viam imaging by use of rapid prototyping model, virtual endoscopy, and patient head 3D-imaging (3D-Doctor) were employed with differential coloration of all substantial head tissues (different tissues visualized in different colors), their anatomic inter-relations, and the extent of pathologic tissue within the operative field. This approach has not yet been used as a standard preoperative or intraoperative procedure in otorhinolaryngology. In this way, we tried to understand the new, visualized 'world of anatomic relations within the patient's head' by creating an impression of perception (virtual perception) of the given position of all elements in a particular anatomic region of the head, which does not exist in the real world (virtual world). This approach was aimed at upgrading diagnostic work-up and surgical therapy by ensuring a faster, safer and above all simpler operative procedure. In conclusion, every ENT specialist, i.e. any member of our surgical team, is able to provide virtual reality (VR)-support in implementing surgical procedures, with additional correct control of all risks, within the limits of surgical normal tissue, without additional trauma to the surrounding tissue in the anatomic region undergoing surgical treatment, while having an impression of the presence in virtual world, navigating through it and manipulating with virtual objects. 3D image analysis and processing, tissue modelling, virtual endoscopy (VE), virtual surgery (VS), the use of rapid prototyping (RP) models in medicine, 3D-computer assisted surgery (3D-CAS), as well as tele-3D-CAS, are a new methods of diagnosis using computer processing of 3D image datasets to provide simulated visualizations of patient specific organs similar or equivalent to those produced by standard 2D-black and white MSCT, MRI images and/or endoscopic procedures, and in the same time represent a basis for various realistic simulations in medicine, and can definitely create an impression of immersion of a physician in a non-existing virtual environment. Visualization avoids the risks associated with real endoscopy, and when used prior to performing an actual endoscopic exam can minimize procedural difficulties and decrease the rate of morbidity, especially for endoscopists in training which was proved in our first 3D-CA-FESS in June 1994, and Tele-3D-CA-FESS in October 1998. If we would like to understand the idea of “virtual reality” (VR), it is necessary to recognize that the “… perception of surrounding world created in our brain is based on information coming from the human senses and with the help of a knowledge that is stored in our brain”. The usual, well known definition says that the impression of being present in a virtual environment, such as VE/tele VE of the patient’s head, that does not exist in reality is called virtual reality (VR). Now, imagine that we can substitute artificially generated sensations for the real standard daily information received by our senses.In this case, the perception system in humans could be deceived, creating an impression of another 'external' world around the man. In this way, we could replace the true reality with the simulated reality that enables precise, safer and faster diagnosis as well as surgery. All systems of simulated reality share the ability to offer the user to move and act within the apparent worlds instead of the real world. The otorhinolaryngologist, e.g., any member of our surgical team, was able to provide VR-support in implementing surgical procedures, with additional correctcontrol of all risks, within the limits of surgical normal tissue, without the additional trauma of surrounding tissue of anatomical region which has undergone surgical treatment, and in the same time they had the impression of presence in the virtual world and could navigate through it and manipulate with virtual objects.

2nd EAORL-HNS, and 2nd CE-ORL, April 2013, Nice, France.
A) Professor Klapan, Instructional Course RHINOLOGY/faculty/invited speaker,
B) EAORL, Nice, France 2013


A) Nives&Ivica Klapan, The Port of Monte Carlo, and B) the Port of Nice, France


A) Plage Beau Rivage, Nice, France, and B) Professor Klapan with Professor Olivier Sterkers,
Hopital Beaujon/Paris/France, the president of the Forum "Robotics", of the 2nd EAORL-HNS, and 2ndCE-ORL
A) Professor Klapan, Instructional Course RHINOLOGY/faculty/invited speaker,
B) EAORL, Nice, France 2013


A) Nives&Ivica Klapan, The Port of Monte Carlo, and B) the Port of Nice, France


A) Plage Beau Rivage, Nice, France, and B) Professor Klapan with Professor Olivier Sterkers,
Hopital Beaujon/Paris/France, the president of the Forum "Robotics", of the 2nd EAORL-HNS, and 2ndCE-ORL













